Metabolomics
Metabolomics
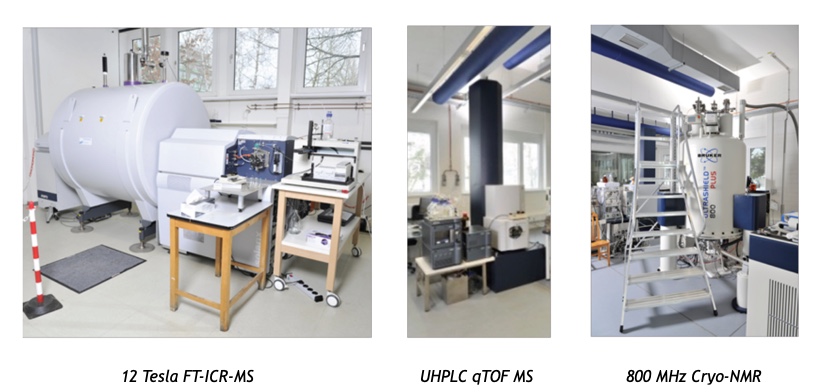
Metabolomics is defined as a comprehensive analysis of all metabolites in a biological system including their identification and quantification [1]. There are different ways to conduct a metabolomics study. Targeted metabolomics experiments focus on metabolite classes (for example short-chain fatty acids) or metabolic pathways (e.g. tryptophan metabolism). In contrast, the non-targeted analysis covers a broad range of metabolites that depend on the technology used such as mass spectrometry or nuclear magnetic resonance spectroscopy. Both techniques have their own strengths but also limitations and are therefore complementary. Non-targeted metabolomics is conducted in various fields of life sciences, exploring the role of metabolites in health and disease. Small molecules can be analysed in various matrices including faeces, urine or plasma across a wide variety of species. Mass spectrometry (MS) is one of the technologies that is used for non-targeted metabolomics, which enables to detect a high number of metabolites with low sample consumption [2].
Blood, urine or stool samples are collected in human metabolomics research to profile metabolites in cross sectional or longitudinal studies of health and diseases. Stool is a valuable proxy of the metabolic state of the gut ecosystem with compounds originating from host, food or microbial metabolism. Previously, metabolomics has been conducted in the context of IBD, where both faecal metabolomics and gut microbiota analysis was performed [3]. But also impact of gut microbiota was studied by non-targeted metabolomics, revealing a large effect of the presence of microbes on plasma metabolome [4]. The application of metabolomics allowed to link three different metabolites of dietary phosphatidylcholine – choline, trimethylamine N-oxide and betaine to predict cardiovascular disease with various functions in atherosclerosis as for example the upregulation of surface receptors on macrophages [5].

Metabolic modelling
While culture-independent approaches for the study of microbial communities have greatly expanded our knowledge of disease-associated shifts in the composition of microbial communities, they are often limited with respect to the inference of functional consequences associated with these shifts. Thus, while species-level changes in gut microbiome composition are observed in the context of almost all human diseases, it is often unclear how these changes affect the functional capacities of the microbiome and, moreover, it is difficult to distinguish which of these changes are potentially part of the disease process and which might only occur as a consequence of disease in the host. Recently, constraint-based metabolic modelling approaches have been developed that are able to overcome some of these limitations. These approaches predict metabolic fluxes (i.e. reaction activities) based on knowledge about the metabolic network of an organism, information on its metabolic environment (i.e. nutrient availability) and additional molecular data (e.g. gene expression data, metabolomics data) [6]. Classically, constraint-based metabolic modelling has been developed to model the metabolism of individual bacterial species [6] or individual cell types of higher organisms [7]. With the recent reconstruction of the metabolic networks of a large number of bacterial species residing in the human gut [8], constraint-based metabolic modelling of the gut microbiome has become possible. To this end, metabolic networks of the individual bacterial species within a microbial community are put into a common simulation environment and metabolic activities of individual bacterial species as well as the metabolic exchange between bacteria and the host can be predicted [911]. Thus, these approaches have already been used to infer functional consequences of species level shifts in community composition in IBD [12] and during the early development of the microbiome in preterm infants [11]. Recently, microbial community modelling has been expanded to also encompass the host, thereby opening up the avenue towards the development of integrated models of microbiome-host interactions [13].

Fiehn, O., Metabolomics–the link between genotypes and phenotypes. Plant Mol Biol, 2002. 48(1-2): p. 155-71. 2. Luan, H., X. Wang, and Z. Cai, Mass spectrometry-based metabolomics: Targeting the crosstalk between gut microbiota and brain in neurodegenerative disorders. Mass Spectrom Rev, 2019. 38(1): p. 22-33. 3. Smirnov, K.S., et al., Challenges of metabolomics in human gut microbiota research. Int J Med Microbiol, 2016. 306(5): p. 266-279. 4. Wikoff, W.R., et al., Metabolomics analysis reveals large effects of gut microflora on mammalian blood metabolites. Proc Natl Acad Sci U S A, 2009. 106(10): p. 3698-703. 5. Wang, Z., et al., Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature, 2011. 472(7341): p. 57-63. 6. Bordbar, A., et al., Constraint-based models predict metabolic and associated cellular functions. Nat Rev Genet, 2014. 15(2): p. 107-20. 7. Thiele, I., et al., A community-driven global reconstruction of human metabolism. Nat Biotechnol, 2013. 31(5): p. 419-25. 8. Magnusdottir, S., et al., Generation of genome-scale metabolic reconstructions for 773 members of the human gut microbiota. Nat Biotechnol, 2017. 35(1): p. 81-89. 9. Gottstein, W., et al., Constraint-based stoichiometric modelling from single organisms to microbial communities. J R Soc Interface, 2016. 13(124). 10. Bauer, E., et al., BacArena: Individual-based metabolic modelling of heterogeneous microbes in complex communities. PLoS Comput Biol, 2017. 13(5): p. e1005544. 11. Graspeuntner, S., et al., Gut dysbiosis with Bacilli dominance and accumulation of fermentation products precedes late-onset sepsis in preterm infants. Clin Infect Dis, 2018. 12. Bauer, E. and I. Thiele, From metagenomic data to personalized in silico microbiotas: predicting dietary supplements for Crohn’s disease. NPJ Syst Biol Appl, 2018. 4: p. 27. 13. Thiele, I., et al., When metabolism meets physiology: Harvey and Harvetta. bioRxiv, 2018: p. 255885.
